- Macular Degeneration
- Dry Macular Degeneration
- AREDS Vitamins
- Amsler Grid
- Wet Macular Degeneration
- Diabetic Retinopathy
- Intravitreal Injections
- Retinal Lasers
- Retinal Surgery
- Flashes and Floaters
At Summit Eye Surgeons, our retina services are designed to address a variety of retinal conditions with the highest level of care and expertise. Led by Dr. Erin Lally, our experienced team offers comprehensive diagnostics and advanced treatments for macular degeneration, diabetic retinopathy, and other retinal disorders. Utilizing state-of-the-art technology, we provide personalized care plans to manage and treat these conditions effectively.
Our goal is to preserve and enhance your vision through meticulous attention to detail and innovative treatment options, ensuring optimal outcomes for our patients.
Macular Degeneration
Age-related macular degeneration (AMD) is one of the leading causes of blindness in the United States in individuals over the age of 60. The macula is the central portion of the retina that has specialized cells which enable color vision and the ability to see fine detail. Cells in the macula can deteriorate with time. When this happens, images are not properly received by the retina and the patient experiences blurred, distorted or missing vision. There are two defined types of macular degeneration: Dry and Wet.

What is Dry Macular Degeneration?
Dry macular degeneration is the most common form of the disease and results in gradual vision loss and distorted vision due to aging of the macula. Dry macular degeneration is characterized by the presence of deposits of cellular waste (drusen) and retinal pigment changes in the central macula. Although the specific causes of dry macular degeneration are unknown, some researchers believe that genetic predispositions and age are factors. Dry macular degeneration is often very slow to progress.
AREDS Vitamins

While there is no cure for dry macular degeneration, a certain vitamin formula has been shown to significantly slow disease progression. The National Institute of Health released the Age-Related Eye Disease Study (AREDS) in 2006, which showed that patients taking the AREDS vitamin supplement were 25% less likely to progress to advanced macular degeneration than patients who received a placebo. In 2013, the vitamin composition was revised (AREDS-2) to include:
- 500mg of Vitamin C
- 400 IU of Vitamin E
- 80mg of Zinc
- 2mg of Copper
- 10mg Lutein
- 2mg Zeaxanthin
Dr. Lally recommends the AREDS-2 vitamin to all individuals with intermediate to advanced macular degeneration. At Summit Eye Surgeons, Dr. Lally will discuss the best treatment plan for your individual needs.
Amsler Grid
A great way to monitor one’s vision and check for early changes in the severity of macular degeneration, is to use an Amsler grid. An Amsler grid is a simple square with a grid pattern and a central dot. To use the Amsler grid, cover one eye and focus the uncovered eye on the central dot and observe the surrounding grid pattern. The user should wear his/her reading glasses and hold the grid at a comfortable reading distance. In patients with a healthy macula, all of the lines should be perfectly straight and there should be no gaps in any line. In patients with macular degeneration, the Amsler grid may appear to have wavy or distorted lines or blank spots. By regularly using the Amsler grid, patients can detect subtle changes in their visual distortions and relay the information to their retinal doctor for further evaluation. If you notice changes in vision on the Amsler grid, call Summit Eye Surgeons for further evaluation.
Wet Macular Degeneration
Wet macular degeneration accounts for roughly 10 percent of patients with macular degeneration. This form of macular degeneration is deemed “wet” due the presence of leakage and bleeding of abnormal blood vessels in the macula. In wet macular degeneration, visual distortions and vision loss tend to be more severe and rapid in onset than the dry variant.
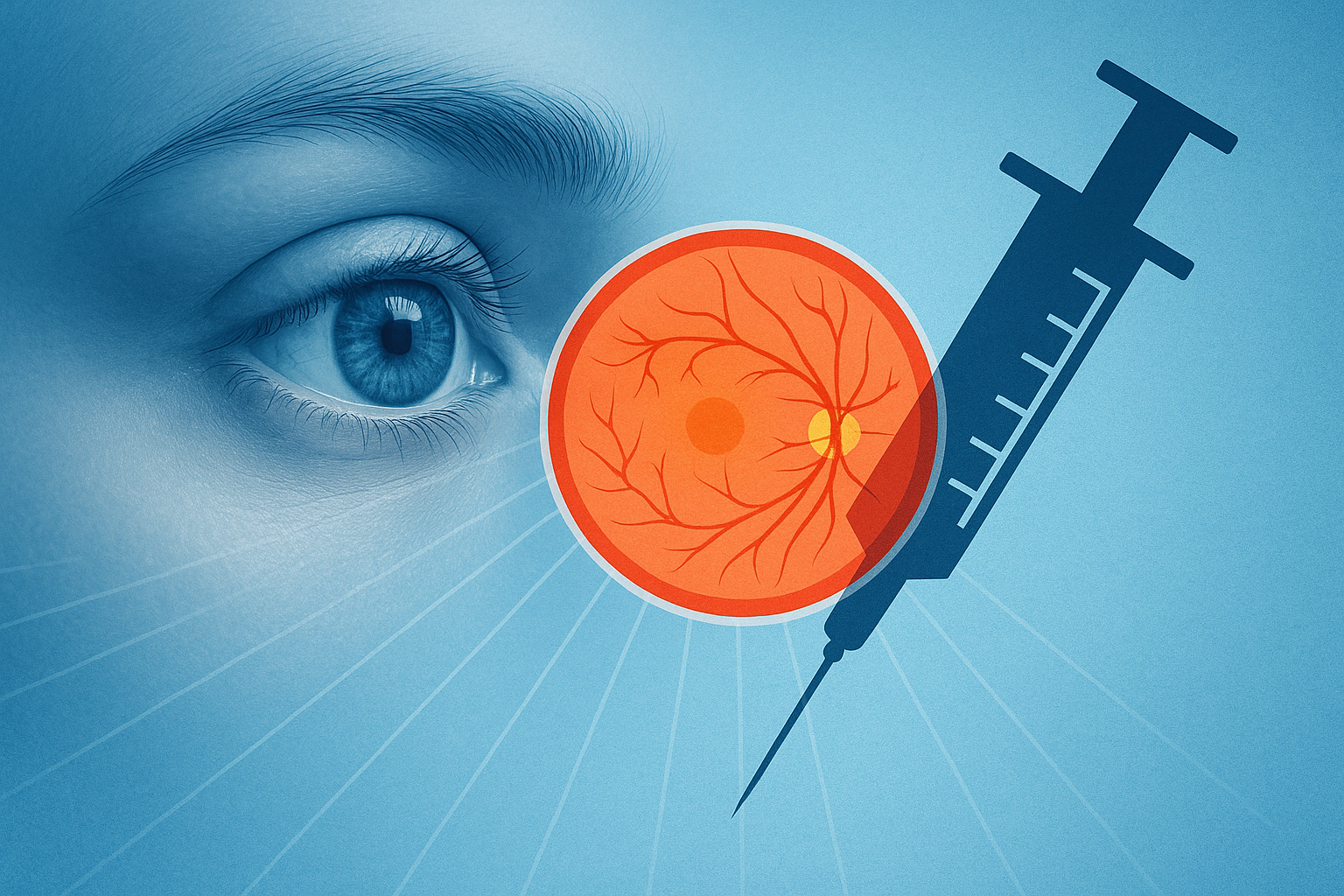
Medications called vascular endothelial growth factor (VEGF) inhibitors (anti-VEGF) can help treat wet macular degeneration. These medications help reduce leakage from abnormal blood vessels. The medication is delivered to the eye using a very slender needle. Prior to giving the medication, the eye is cleaned and numbed with eyedrops. Dr. Lally will determine the type of medication and number of treatments needed to best control the wet macular degeneration.
Call Summit Eye Surgeons for an appointment with Dr. Lally if you or a loved one are concerned about macular degeneration.
Diabetic Retinopathy

Diabetic retinopathy is a complication of diabetes and is the leading reason for vision loss in diabetic patients.
In diabetic patients, high sugar (glucose) levels damage blood vessels in every organ in the body, including the retina. The retina is unique in that it is the only organ in the body where doctors can visualize the vessels and assess for damage. These damaged blood vessels often leak and bleed, causing swelling of the central retina, called macular edema.
In a process called neovascularization, new, fragile and poorly functioning blood vessels grow in the retina which can result in bleeding, retinal detachments and severe glaucoma. Both macular edema and neovascularization of the retina can result in decreased vision, visual distortions and sometimes even loss of vision.
Intravitreal Injections
Intravitreal injections have become the standard of care in treating macular edema. Highly specialized, FDA-approved medications called vascular endothelial growth factor (VEGF) inhibitors and/or steroids can be injected into the eye using a very thin needle to stabilize leaking vessels that are damaged by diabetic retinopathy.
The eye is numbed prior to the injection with topical eye drops. A slender needle is used to inject the medication through the white part of the eye. The injection takes only a few seconds and is performed in the office. The frequency and duration of treatment is determined by a number of factors, including the patient’s initial clarity of vision, severity of diabetic retinopathy, and the patient’s level of glucose control.
Retinal Lasers
Retinal laser surgery (Panretinal Photocoagulation) is often recommended for patients with neovascular retinopathy. The goal of treatment is to prevent further loss of vision by preventing new blood vessels from growing and to shrink the abnormal blood vessels that are already growing.
A different type of laser surgery (Focal laser) can help treat and prevent macular swelling targeting leaky vessels in the macula.
Retinal Surgery
Retinal surgery for diabetes is often reserved for severe cases of diabetic retinopathy in which part or all of the retina has detached and/or the eye has filled with blood. Surgical procedures are performed in an operating room, using microsurgical instruments.
All patients with diabetes should have a dilated retinal examination with an ophthalmologist at least once per year. More frequent eye exams are warranted if retinopathy is detected. At Summit Eye Surgeons, Dr. Lally will work with you to diagnose and treat your retinopathy and to help preserve your vision.

Flashes and Floaters
Floaters appear as small specks, dots or cobwebs in one’s visual field. While floaters appear to be in front of the eye, they are actually inside of the eye. The eye is filled with a clear, jelly-like substance called the vitreous. Over time, natural age-related changes cause the vitreous to becomes more liquid and portions of it clump together. What you experience as a “floater” is actually a shadow of a vitreous clump cast onto the retina. If the vitreous gel liquefies enough and separates entirely from the back of the eye, it is called a posterior vitreous detachment (PVD).
Floaters can be quite annoying and bothersome to the patient, as they can interfere with clear vision. However, they are not serious and tend to break-up or settle over time. Only if the floater is debilitating and interfere significantly with a patient’s vision, should surgical intervention be used to remove the vitreous gel.
In addition to floaters, people can also experience quick bursts or flashes of light in their peripheral vision. Flashes are due to the vitreous jelly pulling on the underlying retina. In contrast to flashes that originate in the retina (quick, brief bursts of light), lingering bright spots, patches or lines in one’s vision can be indicative of a migraine aura or other medical conditions.
While flashes and floaters can be due to normal age-related changes to the eye, it is important that the patient has a dilated retinal evaluation to ensure there is not a more serious underlying problem. Sometimes, these symptoms are due to a tear in the retina and/or broken retinal blood vessels, which can require treatment.
Schedule an appointment at Summit Eye Surgeons with Dr. Lally if you are having flashes and/or floaters.
Related Blog Posts
How Anti-VEGF Injections Protect Your Vision

Protecting Your Vision: A Guide to Macular Degeneration and How to Preserve Your Sight




